Credible Science, Incredible Egg
The latest egg nutrition, research and information.
Take a deep dive into
The Facts Behind the Incredible Egg
We’re the science and nutrition education division of the American Egg Board.

Most Popular
Articles
See All >Featured Categories
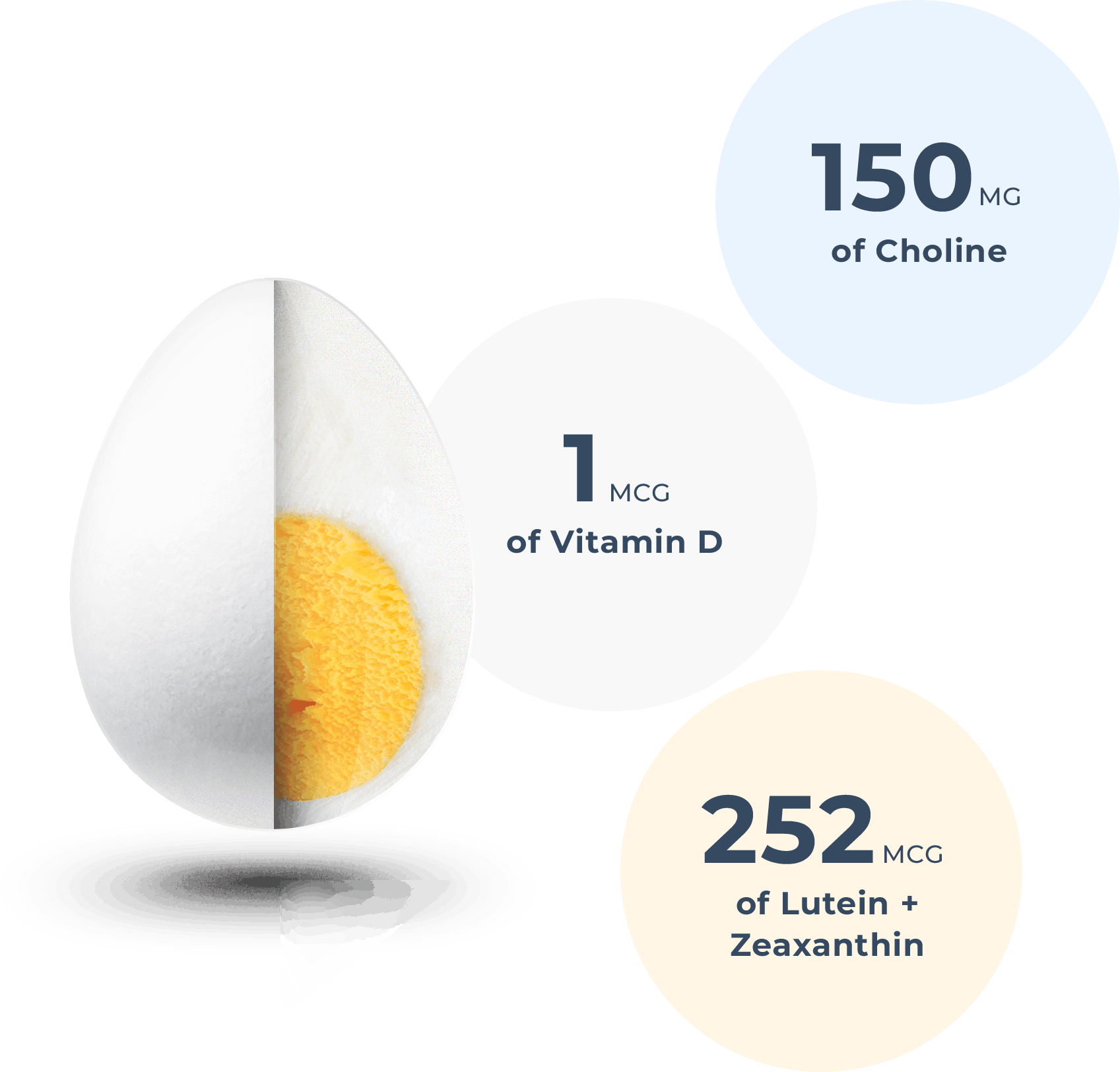
Eggs by the Numbers
Eggs are a nutrient-rich food that provides a good or excellent source of eight essential nutrients. See what else you’ll find in Eggs by the Numbers.
Egg Enthusiast Community
See All >
Veggie, Black Bean, & Egg Quesadilla
Egg quesadillas are one of my fave dishes to make for so many reasons: they’re nutritious, delicious, and affordable! And by adding veggies, we’re getting a great balance of fat, fiber, and protein!
View Recipe titled Veggie, Black Bean, & Egg Quesadilla
Mini Mediterranean Frittatas
Get a taste of the Mediterranean at breakfast with these mini frittatas! Make a batch over the weekend and reheat each morning for a quick and filling breakfast on the go.
View Article titled Mini Mediterranean Frittatas
The Incredible Egg: Cognition, Nutrition & Culinary Hero
Did you know that eggs contain important nutrients for cognition and brain health, including choline and lutein? One large egg contains about 150mg of choline and 252mcg lutein and zeaxanthin. Egg Nutrition Center’s Mickey Rubin, PhD sits down with Melissa Joy Dobbins to chat nutrition, cognition, and all things eggs. Tune into Sound Bites Podcast […]
View Article titled The Incredible Egg: Cognition, Nutrition & Culinary Hero
Avocado Toast Topped With Sunny-Side Egg
Delish #avocadotoast topped with a sunny-side egg hemp seeds, red pepper flakes, lemon olive oil & micro greens
View Social Post titled Avocado Toast Topped With Sunny-Side Egg